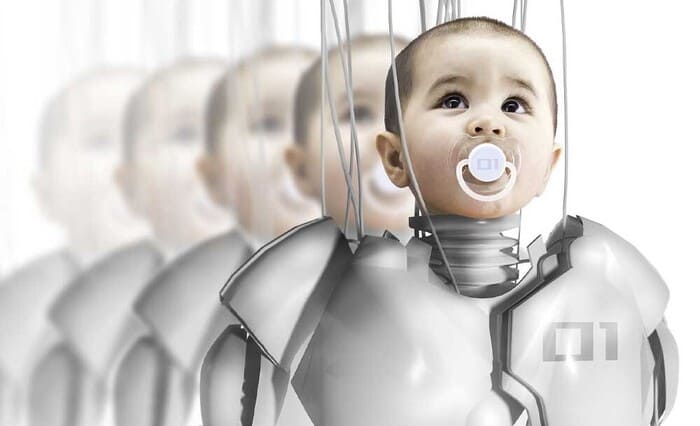
Baby Born by Sperm Injecting Robot: Future of Low-cost IVF Cure
The future of vitro fertilization (IVF) treatment is going to become automated with a robotic sperm-injecting process with successful results.
Yes, a team of engineers in Barcelona, Spain has successfully designed and developed a sperm-injecting robot that has fertilized more than a dozen human eggs, resulting in healthy embryos that successfully give birth to two healthy baby girls.
The robot, which was used by New Hope Fertility Center in New York City, is a prototype that could be used to automate the in vitro fertilization (IVF) process in the future, which would become more accessible and affordable for patients who require it.
Robot Successfully Injected the Sperm
One engineer used a Sony PlayStation 5 controller to position a robotic needle and using a camera, it then moved forward on its own, penetrating the egg and dropping a single sperm cell.
Two healthy embryos eventually turned into two baby girls, who researchers claim are the first ones born after fertilization by a “robot.”
Current IVF Process & Costing
Presently the IVF process is performed manually by trained embryologists who handle eggs and sperm using ultra-thin hollow needles under a microscope.
These labs are quite expensive and have extra maintenance costs. The IVF process is also lengthy, and delicate, and can cost up to $20,000 per attempt in the US.
Currently, around 5,00,000 children are born through IVF each year, but many people don’t have access to fertility medicine or can’t afford it.
Also Read: Biological Father of 550 Children Stopped by Court Donating Sperms
By making IVF more affordable and less labour-intensive, entrepreneurs hope to see a significant increase in the number of children born via IVF in the future.
However, startups such as Overture Life are working towards automating the process, and Overture has raised $37 million from investors to support its work. This cutting-edge procedure could significantly lower the cost of In vitro fertilisation (IVF).
How the Whole Process is done?
A human egg is about 0.1 millimetres across, at the limit of what a human eye can see unaided. Right now, to move one, an embryologist will slurp it up into a hollow needle and squirt it out again.
Inside one of Fertilis’s pods, an egg sits in a chamber no larger than a bead of mist, but the container itself is large enough to pick up with small tongs.
Doctors collect eggs from a woman’s ovaries, they’ll be deposited directly into a micro-cradle and, from there, be nannied by robots until they’re healthy embryos.
Egg collection happens after a patient is treated with fertility hormones. Then a doctor uses a vacuum-powered probe to hoover up eggs that have ripened in the ovaries.
Since they’re floating in liquid debris and encased in protective tissue, an embryologist needs to manually find each one and “denude” it by gently cleaning it with a glass straw.
Tracking the Sperms
Once an egg is in hand, doctors need to match it with a sperm cell. To help them pick the right one, Alejandro Chavez-Badiola, a fertility doctor based in Mexico, started a company, IVF 2.0, that developed software to rank and analyze sperm swimming in a dish.
It’s similar to computer-vision programs that track sports players as they run, collide, and switch directions on a pitch. Here the job is to identify healthy sperm by assessing their shape and seeing how well they swim.
While a person can only keep an eye on a few sperm at one time, a computer doesn’t face that limit. “We humans are good at channeling our attention to a single point. We can assess five or 10 sperm, but you can’t do 50,” says Chavez-Badiola.
His IVF clinic is running a head-to-head study of human- and computer-picked sperm, to see which leads to more babies. So far, the computer holds a small edge.
“We don’t claim it’s better than a human, but we do claim it’s just as good. And it never gets tired. A human has to be good at 8 a.m., after coffee, after having an argument on the phone,” he says.


